The National Health Insurance Authority (NHIA) has reaffirmed its commitment to ensuring efficient healthcare service delivery following the recent uncapping of the National Health Insurance Fund (NHIF).
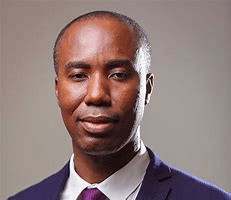
In a statement signed by its Chief Executive Officer, Dr. Victor Asare Bampoe, the NHIA informed all NHIS-credentialed healthcare providers that reimbursement of vetted claims will be processed swiftly and regularly to promote uninterrupted service provision.
“The National Health Insurance Authority (NHIA) wishes to inform all NHIS-credentialed healthcare providers that, following the recent uncapping of the National Health Insurance Fund (NHIF) as announced by the Finance Minister, Hon. Ato Forson MP and in fulfillment of a campaign promise by His Excellency John Dramani Mahama, reimbursement of vetted claims will be made swiftly and on a regular basis, starting this week, to ensure smooth service delivery”
Dr. Victor Asare Bampoe, CEO NHIA
The uncapping of the NHIF marks a crucial milestone in Ghana’s healthcare financing. Over the years, capped allocations to the NHIF have led to erratic reimbursement payments, placing significant financial strain on healthcare facilities.
With this policy shift, the NHIA aims to eliminate delays in claim payments, thereby enabling healthcare providers to operate smoothly and efficiently.
Stakeholders within the health sector have long advocated for uncapping the NHIF, arguing that it would address liquidity constraints faced by service providers and improve patient access to essential healthcare services.

By fulfilling this policy promise, the government has signaled its commitment to prioritizing healthcare financing and ensuring the sustainability of the NHIS.
NHIA’s Expectations from Healthcare Providers
In its official communication, signed by NHIA Chief Executive Dr. Victor Asare Bampoe, the Authority outlined specific expectations for NHIS-credentialed healthcare providers.
The NHIA emphasized the need for strict adherence to policies and regulations, highlighting some critical directives, including the elimination of illegal charges (Co-payment).
Healthcare providers were cautioned against imposing unauthorized fees on NHIS members. The NHIA reiterated its zero-tolerance stance on co-payments, which burden patients and undermine the accessibility of the scheme.

Secondly, the NHIA urged providers to ensure that claims reflect actual patient attendance and adhere to NHIA regulatory standards to curb fraudulent claims and promote financial accountability within the scheme.
Thirdly, healthcare facilities are expected to provide services in accordance with NHIS standards and protocols, ensuring that patients receive the best possible care under the scheme.
To enhance transparency and accountability, the NHIA pledged to continue publishing details of claims payments on its website.
Additionally, monitoring mechanisms will be strengthened to oversee compliance and detect any irregularities in service delivery. Providers found in violation of NHIA policies, particularly those imposing illegal charges, will face stringent sanctions without exception.

As the NHIA implements this policy shift, its success will largely depend on collaboration between the government, healthcare providers, and NHIS members.
Transparency in claims payment, strict enforcement of anti-fraud measures, and adherence to NHIA regulations by service providers will be crucial in ensuring the long-term viability of the NHIS.
Also, additional reforms, such as digitalizing claims processing and enhancing monitoring systems, could further strengthen the scheme.
The uncapping of the NHIF represents a significant step toward achieving universal health coverage in Ghana. However, its impact will depend on sustained government commitment and the cooperation of all stakeholders in the healthcare delivery chain.
READ ALSO: GSE Market Review: Composite Index Dips as Financial Stocks Strengthen